Palliative care for all of Africa The story so far
The birth of Hospice Africa
After a lifetime of clinical experience, working across continents and multiple medical disciplines including Geriatric and Palliative care, Dr Anne Merriman MBE set out on a mission that soon became Hospice Africa. In 1992, the organisation was founded as a charity in Liverpool UK, the birthplace of Dr Anne, with the vision: palliative care for all those in need in Africa.
In order to support the provision of palliative care in Africa, a model hospice was required to provide a service appropriate to the culture and economy, and also offer a training centre for initiators from other African countries. After feasibility studies in four African countries, it became clear that Uganda was the best host country for a centre of excellence. The work of Hospice Africa commenced in September 1993. With funding for only a few months, the two person embryonic team, Dr Anne and Nurse Mbaraka Fazal, were able to make initial progress.

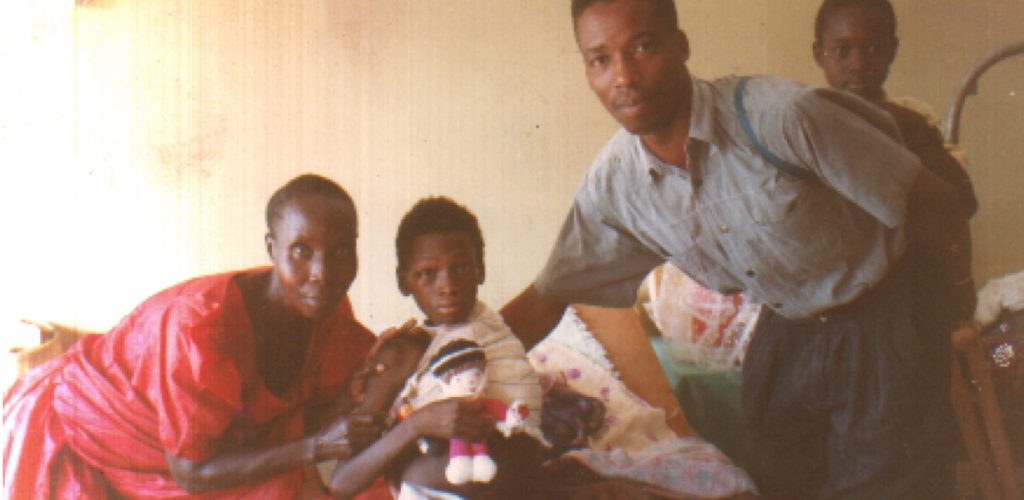
Initial team with donated Land Rover in Ndebba 1994. (from left) Jackson, Betty, Dr Anne, Rose Kiwanuka and Luke.
What is Palliative Care (PC)?
The international definition of palliative care, endorsed by the World Health Organisation (WHO) is:
“Palliative care is the active holistic care of individuals across all ages with serious health-related suffering due to severe illness, and especially of those near the end of life. It aims to improve the quality of life of patients, their families and their care givers.”
More detail from WHO is available HERE

Uganda in the beginning
In 1993 Uganda’s cancer rate was on the increase. Karposi’s Sarcoma, a marker for AIDS, was the most common form of cancer and treatments such as antibiotics or anti fungal agents were scarce and only available for the rich. The pain for those with infections was huge and there was little hope for most patients.
At the time the population of Uganda was 23 million and 57% of the rural population never saw a health worker. As a result, life expectancy was a mere 38 years and HIV prevalence was considered to be 30%. In those first few years, the team saw a lot of very sad cases. A generation of parents was wiped out, leaving children as orphans or being cared for by elderly grandparents.
Access to pain control
One of the most significant steps was the introduction of oral morphine as an affordable painkiller. In 1993, the Minister of Health, Dr James Makumbi, agreed that powdered morphine could be imported, despite the concerns around addiction and criminalisation. This major step, along with the simple recipe for affordable oral morphine that Dr Anne had designed with pharmacists in Singapore and brought with her, allowed the great work of Hospice Africa to grow.
The next issue for the team to tackle was access to this pain relief. In most countries, the only prescribers for Class A drugs are doctors, veterinarians, or dentists and with a severe shortage of doctors in Uganda, there was a real access issue. After a lot of persistence and persuasion from the Hospice team, in 2003 the government finally sanctioned nurses and clinical officers who had received training from Hospice Africa Uganda to prescribe morphine to patients. This breakthrough meant the work of Hospice Africa could be accelerated at a significant rate, resulting in pain relief for hundreds of new patients.
Today, morphine is manufactured at Hospice in Kampala through a public-private partnership with the Ugandan government. The cost is still the price of a loaf of bread for 110 days’ treatment, which serves the needs of an average patient. This allows patients to “live until they die”.

Expansion into rural Uganda
The plan for Hospice Africa involved developing a model of culturally acceptable and affordable palliative care that could be replicated and adapted through multiple organisations across the continent. Although Hospice did not initially envisage setting up other clinics in Uganda, the need to support patients in a more rural setting soon became apparent.
In 1995, the Hospice Africa team were invited to Mbarara to teach palliative care to medical students at the Mbarara University of Science and Technology. It was apparent that this rural part of Uganda had a need for palliative care services, and the momentum began to build. First, the team were kindly donated a Land Rover, driver, and medical supplies, which was enough to get things started. After this came a four- year process of obtaining a large grant which allowed the service to flourish.
Soon the team in Mbarara had a newly refurbished clinic, funding, and the supplies needed to take on many more patients. They were then joined by more doctors and nurses who helped extend the service and later set up outreach and roadside clinics which are so crucial in more rural areas.
The second clinical branch of Hospice Africa was opened in 1998 in Hoima, a rural and sadly neglected town 200km north of Kampala. There was much need for a service to function in this deprived and war-torn part of the country as very little medicine was available to patients suffering from HIV and cancer.
The clinic started from very small premises but eventually received the funding and support it needed to set up a larger centre of its own. Hoima now has access to the full palliative care service of Hospice Africa thanks to our friends, staff, and supporters.
The service in Uganda is now found in 90% of the districts, headed by a registered prescriber trained at HAU. Uganda was the first country in the world to recognise nurse prescribers, following a year’s training to Diploma level in palliative care. This was essential because of the shortage of doctors in Uganda and other African countries.
We work closely with the Cancer programmes at the Uganda Cancer Institute and hospitals. However the majority of Ugandans do not reach these services, so depend on our Community Volunteer Workers (CVW’s) who are trained by us in basic nursing skills and the management of medications. They identify those in need and we then visit these patients at home, with subsequent support provided by our trained CV

Palliative care for all of Africa
To achieve our goal of developing a palliative care network across Africa, our founding members realised the importance of setting up an education department. One year after Hospice Africa was established in Uganda, undergraduate training for nurses, doctors and other healthcare providers commenced. The department grew into what is now the Institute of Hospice and Palliative Care in Africa (IHPCA). Sitting directly alongside Hospice Africa and situated on the same grounds as the clinic in Kampala, IHPCA offers diploma and degree level programs to students across Africa and beyond.
In addition to training at IHPCA, the founding members of Hospice Africa realised the need for a dedicated team to run programs in other African countries, in order to fulfil the mission of providing palliative care for all of Africa. The International Programs team, based in Uganda, connects with partner organisations in other African countries, training healthcare professionals in palliative care practices, meeting with government officials, and advocating the work of Hospice Africa across the continent.
Health professional initiators from other countries are trained at the bedside with our own clinical service in the home and through visits to their countries. Once there, we bring advocacy to the Ministry of Health and the universities, support new services which are affordable and culturally appropriate to each country, and introduce education programmes.

Our mission today
Our mission is to provide a holistic and culturally sensitive palliative care service. This is achieved by opening the door to pain control through accurate treatment of pain and the introduction of affordable oral morphine to each country. This is taken in the home on a regular basis by the patients themselves, closely monitored and recorded following international regulations. With over 37,000 patients treated, we have not experienced any diversion or addiction.
Once pain is controlled, our patients often open up with other worries and anxieties they face approaching the end of life, together with their families. All these are addressed to control “Total Pain” as defined by Dame Cicely Saunders in 1967.
When Hospice Africa arrived in Uganda, there were only three countries in Africa that supplied palliative care. As of 2020 that number is 37, an achievement we are very proud of and thankful for. Although only about 10% of patients in need access palliative care in Uganda, the World Health Organisation and the World Palliative Care Alliance have recognised Uganda as among the countries having the highest palliative care level in the world. Whilst this is an incredible achievement for all that have helped us on our mission, it does highlight how much work remains.
Today, the much needed work and mission of Hospice Africa continues. All across Africa, thousands of our brothers and sisters are suffering from life limiting illness without the adequate pain control that should be their human right. In over our nearly 30 years of operation, we have proven that an affordable and culturally acceptable model is available that can bring peace to those in so much pain.
Although our will to help is burning as fiercely as ever, our funding is inadequate to meet the tremendous need. Large organisations that once provided significant grants to help treat HIV patients have halted funding and today we are feeling the repercussions. Therefore, now more than ever, we need the help of our friends, families, and supporters to keep the work in Uganda and across Africa alive.

